Gluten Antibody Cross-Reactivity in Celiac Disease
When I was first diagnosed with celiac disease, I was told to go gluten-free and I would be totally fine.
So, as much as I didn’t want to give up pizza & beer in second year university, I did.
I replaced all of my dishes, pots, pans, and my roommates were even kind enough to allow me to have a counter-space int he kitchen that was completely gluten-free.
I didn’t eat anything that even “may contain wheat” and if I ate out I would order a salad with chicken, without dressing and specifically request that they pan sear the chicken in a fresh pan, not on the grill where they often toast buns, etc.
I took every precaution I possibly could.
I saw some healing. I gained some of my weight back and my mental health improved. However, after over two years of being strictly gluten-free, my bowel movements were still questionable (I would often still see mucous and undigested vegetables), my hormones were still out of whack (I went 2 years without a period and still hadn’t got it back), and my skin was all over the place.
For years, I pretended these weren’t really problems or that they weren’t related to my disease. Eventually, the need to always know where the nearest bathroom was and my increasing anxiety around food made me put my foot down. I was still unwell and no doctor, or even dietician, seemed to be able to help me.
This is really what fuelled my passion and interest in nutrition and sent me back to school to finally get answers. I wanted to learn the facts and the science and figure out for myself what was holding me back from really healing.
During my studies, I learned a few key things that put the pieces together for me:
1) The damage done over years of undiagnosed celiac disease is significant and may require active steps toward healing rather than just eliminating the damaging substance.
Think of it as if your gut is a brick wall and gluten is a hammer that has been chipping away at it for years. You can get rid of the hammer and that will prevent further damage but unless you do something to patch up the brickwork the damage and holes will remain. For some, it is true that simply removing gluten may allow you to self-heal over time without much added effort, but if you have had celiac for years your body is likely incredibly depleted and without focused nutrition it can be incredibly hard for your body to pull together what it needs to really heal.
2) The autoimmune component of celiac disease needs to be address by way of calming the immune system, balancing the immune system and managing stress.
An autoimmune disease is a condition wherein your own immune system attacks you body’s own tissue. In the case of celiac disease, gluten is the trigger for your immune system to mount this attack. When we remove the gluten, the attack has no trigger and stops. However, the presence of an autoimmune disease indicates that you have an overactive immune system. In order to achieve balance to reduce the autoimmune reaction should you “get glutened” and minimize your likelihood of developing further autoimmune diseases, it is important to address other systems that affect that balance including the nervous system and the endocrine system. We must also support the immune system itself with focused nutrition.
3) There are gluten-free foods that may be able to trigger the same antibodies and therefore, the same autoimmune attack that gluten triggers in celiac disease.
It is estimated that 20% of celiacs do not achieve remission simply by going gluten-free due to cross-reactivity with gluten-free foods. It turns out, anti-gliadin antibodies (the primary antibody reacting to gluten, which is responsible for the autoimmune attack & damage in celiac disease) may also react to certain gluten-free foods, making your body think that it is eating gluten and fuelling the same autoimmune response.
This is the bit I want to focus on today.
How does cross-reactivity happen!?
Stick with me for a minute as I bust through some science. I’m going to try and simplify it as much as possible.
The first thing we need to understand to really comprehend cross-reactivity is that the ONLY thing that antibodies react to are proteins.
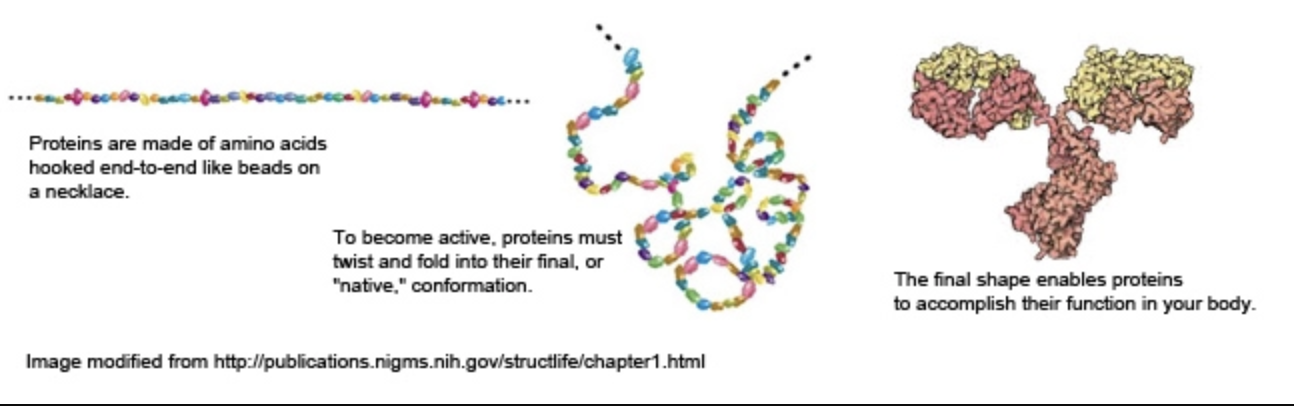
Proteins are all made of long chains of amino acids. Each protein has a different sequence of amino acids which determines what kind of protein is formed. These chains of amino acids fold and buckle in extremely complex ways, giving each protein type it’s individual structure. This structure is allows the protein to perform the functions it is required for.
The next thing we need to understand is that all antibodies are proteins themselves. They are produced by your immune cells, which create sequence of amino acids forms a y-shape. Each tip of the Y is a region of the antibody that can bind to a specific sequence of amino acids within a protein.
NOTE: Remember that it is a specific sequence of amino acids that the antibody binds to, not the whole protein.
Because antibodies bind to that sequence of amino acids and not an entire protein, it is possible for many different antibodies to be formed against one protein or one specific food.
In the case of gluten cross-reactivity, the amino acid sequence that an antibody recognizes is also present in other proteins from other foods that do not actually contain gluten.
Depending on exactly what antibody or antibodies your body forms against gluten, it/they may or may not cross-react with other foods. So, not only are you sensitive to gluten, but your body now recognizes non-gluten containing foods as one and the same.
Which foods might cross-react with gluten?!
A recent study evaluated the potential of gluten cross-reactivity for 24 food antigens. These included:
Cow’s milk
Caesin
Casomorphin
Milk butyrophilin
Whey protein
Milk chocolate
Oats
Brewer’s yeast
Baker’s yeast
Coffee
Sesame
Buckwheat
Sorghum
Millet
Hemp
amaranth
Quinoa
Tapicoa
Teff
Soy
Egg
Corn
Rice
Potato
The Cyrex Labs gluten cross-reactivity blood test looked at two different types of anti-gliadin antibodies (the antibodies that recognize the protein fraction of gluten) finding consistent results with both.
The antibodies did not cross-react to all of these foods but they did cross-react with the following:
All dairy
Cow’s Milk
Casein
Casomorphin
Butyrophilin
Whey
Oats
Baker’s Yeast
Brewer’s Yeast
Instant Coffee (but not fresh coffee!)
Milk chocolate (attributable to the dairy proteins)
Millet
Soy
Corn
Rice
Potato
The figure below was created by Dr. Sarah Ballantyne (aka. The Paleo Mom) to clearly identify the extreme to which the antibodies cross-reacted. The green line indicates the control, identifying that levels below as being negative for gluten cross-reactivity.
SOURCE: The Paleo Mom
This may explain the high frequency of dairy sensitivities in celiac patients. The concern lies especially with the fact that many of us replace gluten with these foods, including rice, corn and millet!
This could be the reason that many of us do not find the healing we expect upon adopting a gluten-free diet. We may still be fuelling the autoimmune disease with these gluten-free foods!
While not all people with celiac disease will be sensitive to all these foods, they may still stimulate the immune system. Just as trace amounts of gluten can cause a reaction, even a small amount of these foods can create inflammation and immune responses that leave us vulnerable to the development of further autoimmune disease and other health concerns.
It is especially important to consider when we think about all the small amounts of things like corn, soy and milk ingredients in even our favourite gluten-free snacks. Even if you think you are avoiding these foods, you could be consuming many of them every single day.
Now, before you totally freak out, even if you do have celiac disease, you may not have these antibodies that will cross-react. If you have gone gluten-free and have seen all of your symptoms resolve, you may be just fine. It is simply worth considering for those who have not seen total remission or still experience other inflammatory symptoms. They may not be unrelated.
If you think you might have cross-reactivity issues, I would consider an elimination/gut healing protocol. It would be best to work with a qualified nutritionist or functional medicine practitioner to eliminate the suspected foods, take steps to heal the gut and calm the immune system and reintroduce each food individually to test for reactivity.
If you are just getting started on a gluten-free diet, I recommend you grab my FREE Quickstart Guide to Going Gluten-Free. This will make sure you have all the basics down, including how to avoid cross-contamination, and set you up with some gluten-free & dairy-free, gut-healing recipes to get you started on the right foot!
When I finally took the extra steps toward actively healing my gut, supporting my immune system, balancing my hormones and avoiding foods that could negatively affect any of those things, I found full remission and have never looked back.
I know it is a lot. It is a huge life change, but it is SO worth it. My quality of life is 100x better. I can enjoy my life and my food WITHOUT anxiety and be confident that I am doing everything I can to avoid further autoimmune diseases or other health complications.
You are worth it.
I am here for your support every step of the way.
Stay tuned here & on instagram @realistic.holistic and always feel free to reach out with questions or requests for additional content. And if you want to work with me independently, please fill out the form here to get in contact with me and we will schedule a discovery call to see if we are the right fit!
As always, thank you so much for stopping by.
Kisses & kombucha,
Meg
SOURCES
Ballantyne, Sarah, et al. “Gluten Cross-Reactivity: How Your Body Can Still Think You're Eating Gluten Even after Giving It up. ~ The Paleo Mom.” The Paleo Mom, 17 Aug. 2018, www.thepaleomom.com/gluten-cross-reactivity-update-how-your-body-can-still-think-youre-eating-gluten-even-after-giving-it-up/.
Mickowska, Barbara, et al. “Oat Raw Materials and Bakery Products - Amino Acid Composition and Celiac Immunoreactivity.” Acta Scientiarum Polonorum. Technologia Alimentaria, U.S. National Library of Medicine, 2016, www.ncbi.nlm.nih.gov/pubmed/28071042.
“The Structures of Life.” National Institute of General Medical Sciences, U.S. Department of Health and Human Services, www.nigms.nih.gov/education/Booklets/The-Structures-of-Life/Pages/Home.aspx.
Thompson, Tricia, et al. “Gluten Contamination of Grains, Seeds, and Flours in the United States: a Pilot Study.” Journal of the American Dietetic Association, U.S. National Library of Medicine, June 2010, www.ncbi.nlm.nih.gov/pubmed/20497786.
Vojdani, Aristo, and Igal Tarash. “Cross-Reaction between Gliadin and Different Food and Tissue Antigens.” Food and Nutrition Sciences, Scientific Research Publishing, 10 Jan. 2013, www.scirp.org/journal/PaperInformation.aspx?PaperID=26626.
Cyrex Labs Array 4: http://www.cyrexlabs.com/CyrexTestsArrays/tabid/136/Default.aspx
Image of antibody binding taken from: http://classes.midlandstech.edu/carterp/Courses/bio225/chap17/ss2.htm